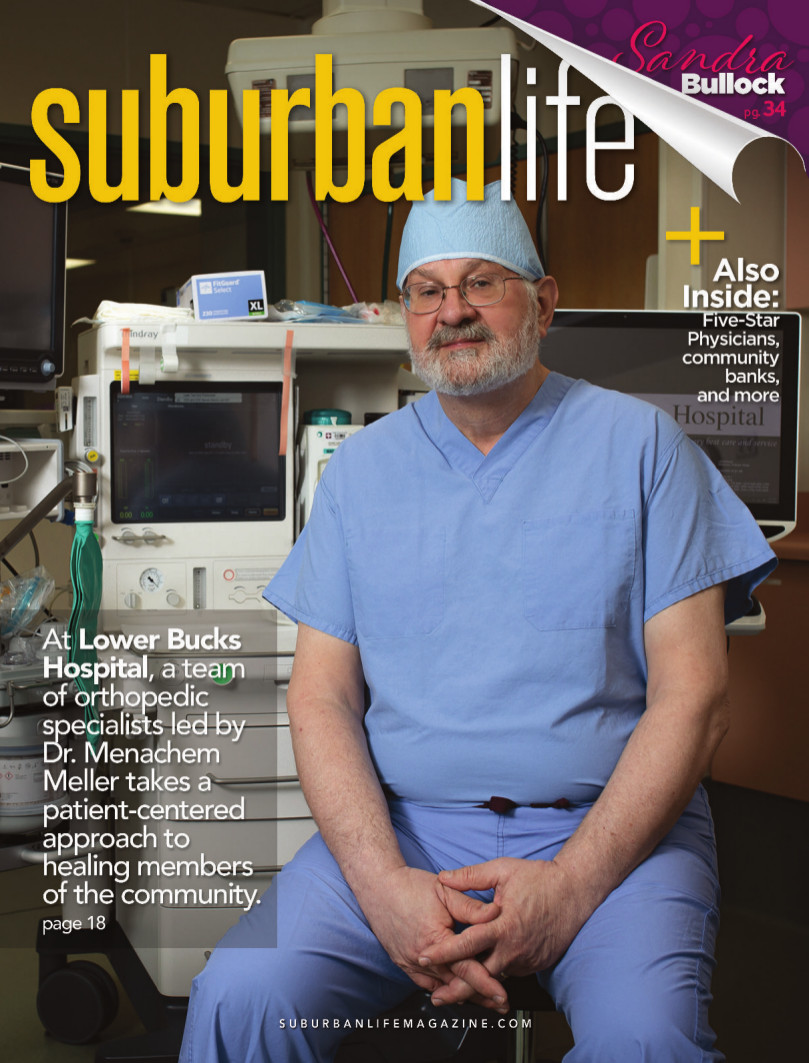
Fully Mended
At Lower Bucks Hospital, a team of orthopedic specialists led by Dr. Menachem Meller takes a patient-centered approach to healing members of the community.
Whereas some people struggle to find their calling, Menachem M. Meller, M.D., Ph.D., FAAOS, has always been clear-eyed about what he wanted to do with his life.
Blessed with a curious mind, an inclination toward all things mechanical, and a desire to make a difference in the world, Dr. Meller began his career as an engineer. Specifically, he worked on a team tasked with developing synthetic fuels to address the nation’s energy crisis. Once he came to the realization that the world was not yet ready to move away from traditional fossil fuels, however, he began pursuing another avocation that would not only suit his mechanical interests but also enable him to help others.
He found the answer in orthopedic medicine, the art and science of using both surgical and nonsurgical interventions to address various ailments of the human musculoskeletal system.
“I was drawn to the engineering aspects of musculoskeletal care, but I also really wanted to do something that would help people,” he says. “To me, everything comes back to patient-centered care, which is a concept that people equate with quality. Quality is easier to define in orthopedic medicine than it is in other areas of medicine because it usually involves a problem-focused interaction. Someone comes in with a broken wrist, and it’s my job to help them heal, restore function, and minimize their pain so they can return to where they were prior to the injury.”
Dr. Meller, who grew up in Brooklyn, is a board-certified orthopedic surgeon who serves Lower Bucks Hospital as section chief of orthopedic surgery. He began his medical education at Brown University in Providence, Rhode Island, and earned his medical doctorate at Rush Medical College in Chicago. Upon graduation, he completed his internship and residency at hospitals in Philadelphia. He spent several years as an orthopedic surgeon with community hospitals and medical centers in Philadelphia until January 2020, when he joined Lower Bucks Hospital.
“Lower Bucks is a community hospital, also called a critical access hospital, and we have access to the same types of treatments some of the bigger-brother institutions provide,” he says. “Rather than a specialty practice, we’re a community-based practice. That means we provide whatever the community needs. I feel very fortunate to work in this environment, offering patient-centered care to people who need it. I spend most of my days talking to patients, listening to their needs, and trying to tailor recommendations to what is safe, effective, and appropriate for that individual.”
Emergency care is vital to a community-based hospital, which is why Dr. Meller begins and ends each day alongside his fellow care providers in Lower Bucks Hospital’s emergency department. Some patients who come into the emergency department with orthopedic issues will require surgical intervention, though many are better served by nonoperative treatment. Dr. Meller says Lower Bucks Hospital has the same goal regardless of the patient’s specific need: “to ensure timely and appropriate musculoskeletal care.”
“Same-day care is about timeliness and effective treatment, but it’s much more than that,” he adds. “The same person who treats you has to understand you and look out for your best interests. Are they asking questions about aspects of your life and health unrelated to the fracture? Are they discussing whether you have weak bones and may be at risk for another fracture? Are they treating you with dignity, respect, and common sense?”
For patients who do require orthopedic surgery, Dr. Meller says knee, hip, and shoulder arthroplasty (joint replacement) has evolved considerably since he first started practicing. Continued advances in surgical technology and technique, materials durability, and perioperative management, for example, have combined to foster better, longer-lasting surgical outcomes. Surgeons have altered their advice to patients, too.
“Years ago, a hip or knee replacement was meant to last 10 or 15 years, so our advice was to wait until you could no longer stand the pain,” Dr. Meller says. “You would start the clock later in life so the replacement would last the patient for the duration of their lifetime. Now that the implant and the technology have improved, the expectation is for the surgical result to last 30 years or more.
“Under those circumstances,” he continues, “there is no reason to wait until the pain and suffering get so bad that you can’t stand it anymore. Now our advice is to wait until your knee or hip is sufficiently painful or disabling, or sufficiently interfering with your daily needs, your occupation, or other activities.”
Another significant perioperative shift involves pain management. Postoperative pain may be commonplace after joint-replacement surgery, but many surgeons have chosen to limit prescriptions for potentially addictive opioid medications in favor of appropriate multimodal therapy, to include over-the-counter pain relievers.
Dr. Meller believes limiting the use of opioids can help combat the opioid epidemic, which has touched almost every American family in some way. From November 2020 to November 2021, more than 106,800 Americans died from drug overdose, according to the U.S. Centers for Disease Control and Prevention—the eighth straight year with more than 100,000 opioid-related deaths.
Also, as opposed to the previous and more conservative approach to postoperative mobility, surgeons now strive to get patients up and moving shortly after surgery. Doing so not only kickstarts the healing process but also speeds up the patient’s ability to achieve his or her ultimate goal—returning to the comforts of home and normal life.
“Any time someone comes to the hospital, they are bound to face some not-so-positive aspects of the experience—the most painful of which is probably dealing with insurance companies,” Dr. Meller says. “We try to make the experience as positive as possible. With the advent of patient-reported outcome measures, as well as objective outcome scores, we are able to focus on timely interventions, early mobilization, minimized discomfort, and minimized hospital admissions and complications.
“A lot has changed since I first started practicing medicine,” he continues. “What has not changed is my approach to working with patients. I always look out for patients’ best interests, and treat them with dignity, respect, and realistic goals. My primary goal is to take care of people, and that’s something that’s never going to change.”
Lower Bucks Hospital
501 Bath Road
Bristol, PA 19007
(215) 785-9200
www.lowerbuckshosp.com
501 Bath Road
Bristol, PA 19007
(215) 785-9200
www.lowerbuckshosp.com
Photograph by Gabriela Barrantes
Published (and copyrighted) in Suburban Life magazine, May 2022.