Dental Implants: Are You a Viable Candidate?
Existing medical issues and other factors can affect the success of dental implants. Here’s what you should know.
Dental Implants have become the standard care of rehabilitation of missing teeth. Since the concept of osseointegration was introduced nearly 50 years ago, implant dentistry has developed into a successful and predictable treatment modality for replacing missing teeth.
Dental implants have gained popularity because, in contrast to other treatment modalities, they preserve adjacent tooth structure and bone. Implant rehabilitation for patients who are edentulous (missing teeth) and partially edentulous report enhanced masticatory function and quality of life.
Three million people already have dental implants in the United States, according to the American Academy of Implant Dentistry. Considering the increased number of dental implants being placed, there are a few things that you, as a dental consumer, need to review with your dental care provider to ensure that you are a viable dental implant candidate.
* Age. Studies have shown that elderly patients are more prone to systemic diseases and comorbidities. They also have potentially longer healing periods, more challenging bone conditions (quality and quantity), increased susceptibility to drug interactions, and increased dental implant morbidity. In addition, decreased renal function, decreased gastric motility, and isolated systemic hypertension are all potential medical issues. Age is most certainly a prognostic factor in implant failure and morbidity. However, advanced age is not an absolute contraindication to implant therapy.
* Antidepressants. For patients with anxiety/depression, medications known as selective serotonin reuptake inhibitors (SSRIs) affect bone metabolism and, therefore, affect the density of the bone surrounding the implant.
* PPIs for patients with gastroesophageal reflux disease, or GERD. Proton pump inhibitors (PPIs) are responsible for the breakdown and absorption of vitamins and nutrients such as vitamin B12, iron, calcium, and magnesium. Because of the decrease in the available nutrients and vitamins, bone metabolism is negatively affected and results in a decrease in bone density.
* Methotrexate for patients with rheumatoid arthritis (RA). RA is an autoimmune disease that causes inflammation, synovial thickening, edema, joint pain, and eventual bone mineral dissolution. Affecting women to men by a ratio of 3:1, the disease affects an estimated 1.5 million Americans. RA patients also have been susceptible to developing osteopenia/osteoporosis in 25 percent to 60 percent of the cases with or without the use of steroids.
* Diabetes mellitus. A chronic medical condition that has reached epidemic proportions throughout the world, diabetes occurs when the body’s ability to produce or respond to the hormone insulin is impaired, thereby increasing the concentration of glucose in the blood. Elevated levels of glucose have been associated with micro- and macro-vascular complications that may result in increased tooth loss, periodontitis, bone-graft failure, implant failure, and peri-implant disease. Therefore, it is imperative that the implant clinician determines the glycemic control of diabetic patients prior to treatment. Ideal HbA1c values for diabetics is 6 percent, with glycemic control in the range of 6 percent to 7 percent. An increased failure rate of dental implants has been associated with poor metabolic control.
* Thyroid disorders. The second-most common endocrine problem affects approximately 1 percent of the general population, principally women. Decreased levels of T4 (thyroxine) affect bone metabolism by decreasing recruitment and maturation of bone cells, and therefore reduce bone-growth factors such as insulin-like growth factor.
* Hyperparathyroidism. This condition stems from an excess of parathyroid hormone (PTH) in the bloodstream caused by overactivity of one or more of the parathyroid glands that maintain calcium balance. This results in altered trabecular bone patterns, mobility of teeth, and compromised bone density. Dental implants and bone grafting are contraindicated (absolute) in areas of active bony lesions resulting from hyperparathyroidism.
* Osteoporosis. The most common disease of bone metabolism an implant clinician will encounter is an age-related disorder characterized by a decrease in bone mass, increased micro-architectural deterioration, and susceptibility to fractures. A strong correlation has been shown between peri-implant disease and skeletal osteoporotic changes.
* Fibrous dysplasia (FD). FD is a nonheritable genetic disorder characterized by normal bone being replaced by immature, haphazardly distributed bone and fibrous tissues. Healing after bone surgery in patients with FD is much different than for those with normal bone, resulting in slower healing and an increased infection rate that may spread throughout the bone and result in more advanced complications.
* Osteomalacia. Osteomalacia is directly related to calcium deficiencies and results in less dense bone. Vitamin D is synthesized by the body in several steps involving the skin, liver, kidneys, and intestines. The kidneys, in conjunction with PTH, activates vitamin D. With this deficiency, the intestinal uptake and mobilization of calcium from the bone is altered, resulting in hypocalcemia. This will lead to an increased PTH secretion, which increases the clearance of phosphorus, resulting in a decrease in the normal mineralization process.
* Xerostomia. Also known as dry mouth, xerostomia may have direct or indirect effects on dental implants and bone-grafting procedures. This results in increased biofilm (plaque) formation, which creates a favorable environment for bacterial growth.
* Radiation therapy for head and neck cancer. Although the survival rate of patients with head and neck cancer has increased over the last 20 years, it remains one of the deadliest forms of cancer. Aggressive treatment includes surgery, radiation, chemotherapy, or a combination therapy that inevitably leaves the patient with compromised anatomy and physiologic functioning. This results in changes in the vascularity and cellularity of hard and soft tissue, damage to the salivary glands, and increased collagen synthesis that results in fibrosis. Because of these detrimental effects on the bone, wound repair and healing are significantly reduced after surgical procedures. When exposed to high levels of radiation, bone undergoes irreversible physiologic changes that include narrowing of the vascular channels (endarteritis), diminished blood flow, and loss of osteocytes. This results in the bone becoming non-vital, which leads to limited remodeling and healing potential.
* Autoimmune diseases such as Sjögren’s syndrome, systemic lupus erythematosus, and scleroderma. These patients are placed on immunosuppressants, steroids, and nonsteroidal anti-inflammatory medications that can influence bone health and implant stability.
Studies have found that the early loss of implants is common among patients with co-existing medical conditions such as the ones I have outlined here. Patients need to carefully review all their health history with their dental implant provider. Furthermore, they should be thoroughly evaluated for their dental health and medical health and any issues must be amended prior to any implant surgery if there is to be a successful outcome.
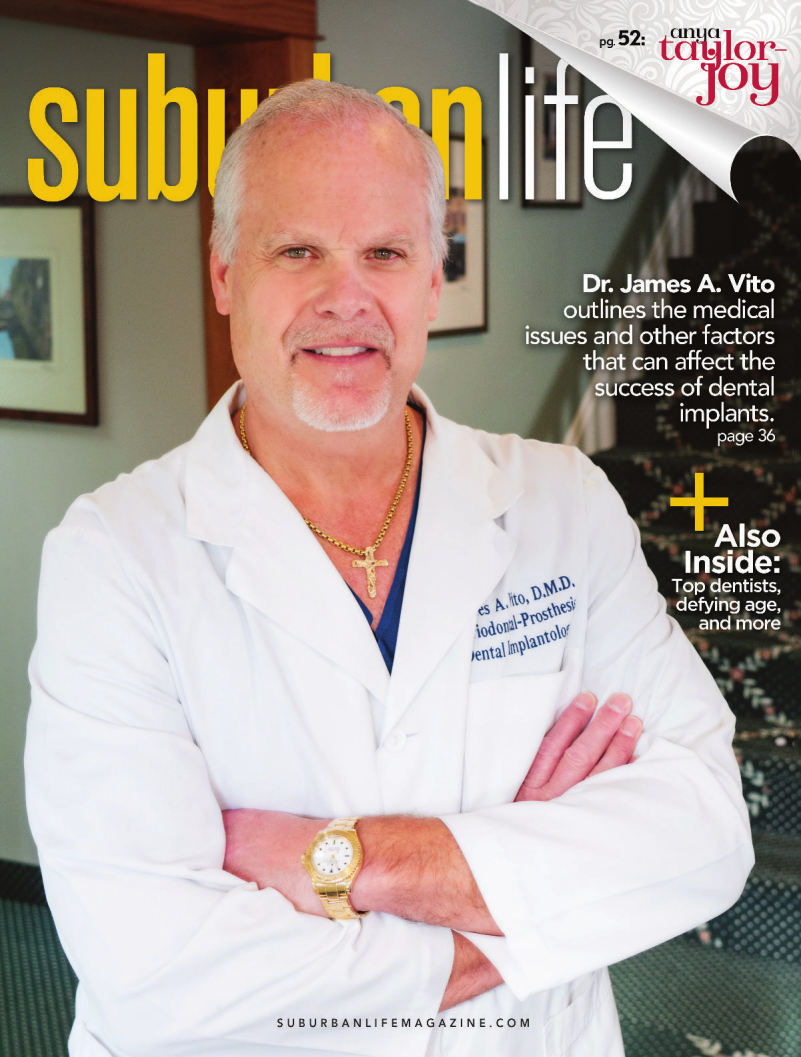
About Dr. Vito
Dr. Vito is a dental implant surgeon and implant restorative dentist who is board certified by both the International Congress of Oral Implantologists and the American Board of Oral Implantology. He received his training as both a periodontist and periodontal prosthodontist from the University of Pennsylvania School of Dental Medicine in Philadelphia.
Dr. Vito is a dental implant surgeon and implant restorative dentist who is board certified by both the International Congress of Oral Implantologists and the American Board of Oral Implantology. He received his training as both a periodontist and periodontal prosthodontist from the University of Pennsylvania School of Dental Medicine in Philadelphia.
James A. Vito, D.M.D.
523 E. Lancaster Ave.
Wayne PA 19087
(610) 971-2590
www.jamesvito.com
523 E. Lancaster Ave.
Wayne PA 19087
(610) 971-2590
www.jamesvito.com
Photo by Jeff Anderson
Published (and copyrighted) in Suburban Life magazine, January 2023.
Published (and copyrighted) in Suburban Life magazine, January 2023.