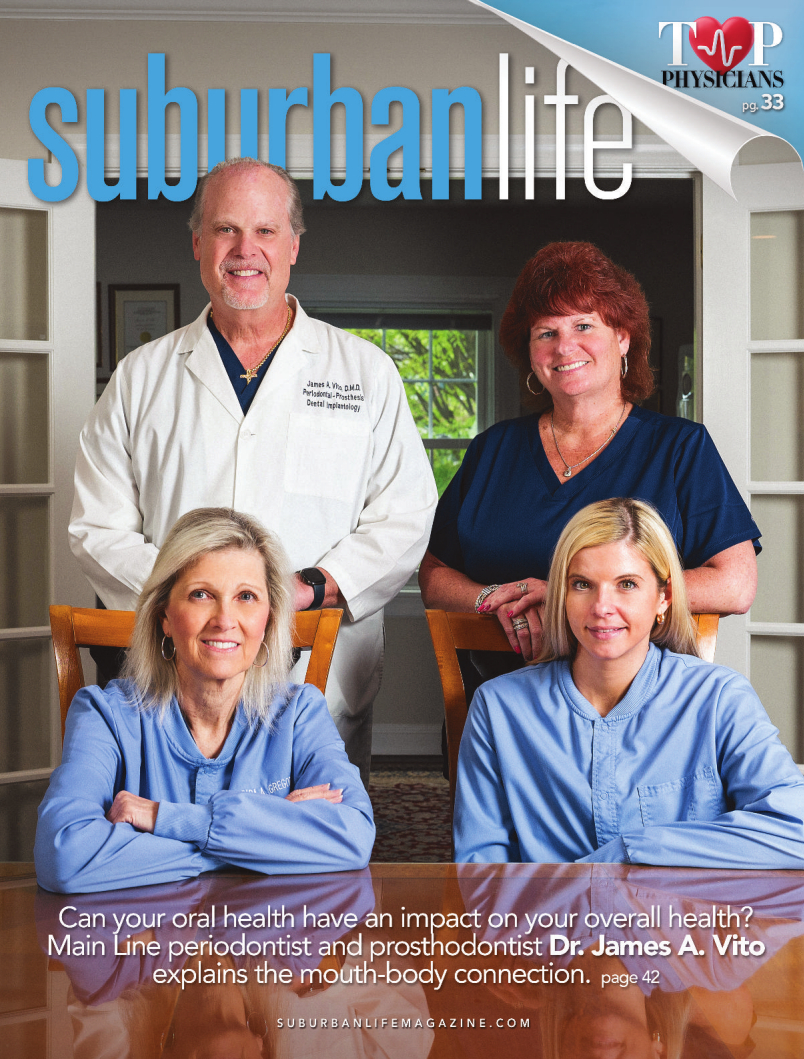
Illuminating the Mouth-Body Connection
How can your oral health affect your overall health? Main Line periodontist and prosthodontist Dr. James A. Vito explains.
What is the importance of good oral health? Simply put, poor oral health can have a profound impact on your overall health, and also complicate some medical issues.
Good oral health can help control and/or lessen the risk associated with heart disease, diabetes, pregnancy, and other conditions. It can also improve self-esteem because healthy teeth and gums are important to how people feel about themselves. Good oral health lets you speak clearly; taste, chew, and swallow delicious and nutritious foods; and show your feelings through facial expressions such as smiling. It is essential for communication, human relationships, and financial prosperity.
Conversely, poor dental health has serious consequences, including painful, disabling, and costly health conditions. Beyond unsightly smiles and bad breath, research from the Oral Health Foundation shows that dental problems can contribute to several chronic conditions: heart problems, strokes, diabetes, premature and low-birth-weight babies, lung disease, Alzheimer’s disease and other forms of dementia, cancer, and a shorter lifespan.
HEART PROBLEMS: People with poor oral health have an increased risk of heart attack and stroke, coronary heart disease, cardiac arrhythmia, and heart failure. People with heart valve disease are particularly at risk when gum disease is present, according to Marietta Ambrose, M.D., assistant professor of clinical Medicine at the University of Pennsylvania’s Perelman School of Medicine.
“The bacteria that live in your mouth when you have gum disease can cross into your bloodstream, enter the heart, and directly infect the vulnerable heart valves,” Dr. Ambrose says. “That’s especially concerning in our patients who have artificial heart valves.”
Infections in the bloodstream, especially those that affect the heart valves, need immediate attention from a cardiologist.
STROKES: Studies have shown that gum disease, missing teeth, and other signs of poor oral health, as well as poor brushing habits and lack of plaque removal, increase stroke risk. According to the American Stroke Association, stroke is the fifth-leading cause of death and a leading cause of disability in the United States. Previous research has also found that gum disease and other oral health concerns are linked to heart disease risk factors and other conditions like high blood pressure.
“What hasn’t been clear is whether poor oral health affected brain health, meaning the functional status of a person’s brain, which we are now able to understand better using neuroimaging tools such as magnetic resonance imaging or MRI,” says Cyprien Rivier, M.D., a postdoctoral fellow in neurology at the Yale School of Medicine. “Studying oral health is especially important because poor oral health happens frequently and is an easily modifiable risk factor.”
DIABETES: Diabetes is a condition that happens when your blood sugar (glucose) is too high. It develops when your pancreas doesn’t make enough insulin or any at all, or when your body isn’t responding to the effects of insulin properly. Diabetes affects people of all ages. Most forms of diabetes are chronic (lifelong), and all forms are manageable with medications and/or lifestyle changes. Many things can cause high blood sugar (hyperglycemia), including sickness, stress, overeating, and not taking enough insulin. People with diabetes face a higher risk of:
* Dry mouth: Unmanaged diabetes can decrease saliva (spit) flow, resulting in dry mouth. Dry mouth can further lead to soreness, ulcers, infections and tooth decay.
* Gum inflammation (gingivitis) and periodontitis: Diabetes not only weakens white blood cells but also causes blood vessels to thicken. This slows the flow of nutrients and waste products throughout the body, including the mouth. As a result, the body loses its ability to fight infections. Because periodontal disease is a bacterial infection, people with unmanaged diabetes might experience more frequent and more severe gum disease.
* Poor healing of oral tissues: People with unmanaged diabetes do not heal quickly after oral surgery or other dental procedures because blood flow to the treatment site can be compromised.
* Thrush: People with diabetes who frequently take antibiotics to fight various infections are especially prone to developing a fungal infection of the mouth and tongue. The fungus thrives on the high glucose levels in the saliva of people with unmanaged diabetes. Wearing dentures (especially when they are worn constantly) can also lead to fungal infections. The presence of thrush can also cause burning mouth syndrome.
People with diabetes who smoke are at an even higher risk—up to 20 times more likely than non-smokers—of developing thrush and periodontal disease. Smoking also seems to impair blood flow to the gums, which might affect wound healing in this tissue area.
PREMATURE AND LOW-BIRTH-WEIGHT BABIES: Pregnancy is a good reason to take extra care of your body, including the mouth. “The thought is that oral bacteria can travel into the bloodstream and cause harm to the fetus,” says Sasha Ross, D.M.D., a periodontist at the Cleveland Clinic. In pregnant women, poor oral health is associated with fetal growth restriction, gestational diabetes, low birth weight, miscarriage, stillbirth, and preeclampsia.
LUNG DISEASE: A number of theories have been put forward with regards to oral health and lung disease. These can be summarized as follows:
* Oral bacteria that colonize the oropharynx may be aspirated through the lower respiratory tract, particularly in individuals at high risk of infection, such as hospitalized patients.
* Salivary enzymes associated with periodontal disease may modify the mucosal surfaces along the respiratory tract, thus facilitating colonization by pathogens.
* Hydrolytic enzymes resulting from periodontal disease may destroy salivary films and consequently make bacteria elimination difficult, thus promoting the possibility of aspiration of these pathogens into the lungs.
* Inflammatory molecules and peripheral mononuclear cells present in saliva may modify the respiratory epithelium and promote colonization by respiratory pathogens.
Although the association is not fully established and the biological mechanisms not yet fully understood, it is important to realize that oral diseases are preventable and protocols should be developed to prevent the possibility of such an association.
ALZHEIMER’S AND DEMENTIA: Researchers have acknowledged for decades the connection between a healthy body and a healthy mind. Recent research is extending that link to draw a connection between oral health and Alzheimer’s disease and dementia.
A recent analysis led by National Institute on Aging (NIA) scientists suggests that the bacteria associated with periodontal disease that causes the chronic inflammation of the gums are also associated with the development of Alzheimer’s disease and related dementias, especially vascular dementia. The results were reported in the Journal of Alzheimer’s Disease.
The NIA Intramural Research Program team used nationally representative, publicly available data from the National Health and Nutrition Examination Survey (NHANES), a large population study performed by the U.S. Centers for Disease Control and Prevention’s National Center for Health Statistics. The team used restricted data linkages with Medicare records and the National Death Index to examine whether the bacteria associated with periodontal infections were linked to dementia diagnoses and deaths. The team compared different age groups at baseline, with up to 26 years of follow-up, for more than 6,000 participants. The analysis revealed that older adults with signs of periodontitis at baseline were more likely to develop Alzheimer’s during the study period.
CANCER: Poor oral health can also lead to an elevated risk of pancreatic cancer, kidney cancer, and blood cancers. Patients with gum disease will typically have weaker immune systems, and are more susceptible to infection.
SHORTER LIFE SPAN: Research reveals that people who live 100 years or more lose fewer teeth during their lifetime. This is because oral health mirrors our overall health, and scientific evidence highlights that people with more than 20 healthy teeth have a 2.5 percent lower death rate.
Medicine sees the impact oral health has on overall health—and you should, too. By protecting your oral health with good oral hygiene (daily brushing and flossing, as well as keeping regularly scheduled dental appointments), the odds are in your favor that you can keep your teeth—and help protect your overall health—for a lifetime.
James A. Vito, D.M.D.
523 E. Lancaster Ave
Wayne, PA 19087
(610) 971-2590
www.jamesvito.com
523 E. Lancaster Ave
Wayne, PA 19087
(610) 971-2590
www.jamesvito.com
Photo by Jeff Anderson
Published (and copyrighted) in Suburban Life magazine, August 2024.
Published (and copyrighted) in Suburban Life magazine, August 2024.